I’ve been a physician in rural Kansas for over fifteen years, and I am extremely fearful for my patients’ health right now. Medicaid is the backbone of healthcare in rural communities. It’s how working families, seniors, and people with disabilities are able to see a doctor, get their medications, and receive lifesaving care. But with massive cuts to this essential program on the horizon, I keep thinking about my patients. How long will they be able to afford the care they need – and what will happen when they no longer can?
Patients won’t be able to afford care without Medicaid
When I moved to Fredonia in 2009, Fredonia Regional Hospital was serving (and still does) all of Wilson County and the surrounding counties. There’s no shortage of patients who need care. But like many rural counties, many of the people we treat are on Medicaid. And the majority of them are kids.
In fact, Medicaid covers about 32% of Kansas children in rural areas. That means that when I treat kids for everything from annual checkups to broken bones, 1 in 3 of them depend on Medicaid to just walk through the door. And as a parent, I know how often our kids need to see a doctor. Without Medicaid, many of my families would simply not get care.
Recent cuts to Medicaid will put their lives at risk. Over the next 10 years, 13,000 Kansans will lose their healthcare, forcing them to pay out of pocket. Most people can’t afford their medical bills with insurance, let alone without it. Without Medicaid, these families will avoid care as long as possible, knowing they can’t pay these massive bills without going in the hole. Kids will get sicker, they’ll miss more school, and their futures will be impacted.
Rural hospitals will be forced to close, putting lives at risk
87% of Kansas hospitals are regularly losing money. Naturally, I thought about what would happen if my community lost its hospital, but more importantly, how my patients would get care. Our hospital serves the entire county and surrounding areas. The next closest emergency room is 15 miles away. Just because we live in a rural area doesn’t mean our lives are worth less, that our care should be put on the back burner.
But it’s not just my community that could lose access to care. A report from the Center for Healthcare Quality and Payment Reform showed that 63% of Kansas hospitals were at risk of closing. Guess how many of them were in rural parts of our state? Every single one. And with the devastating cuts that legislators voted for this summer, it’s safe to assume that many of those hospitals will be gone in the next decade.
It will hurt Kansas families, communities, and our economy
It’s more than people losing care – they’re losing jobs too. Hospitals are major employers, especially in less populated areas. Kansas hospitals provide 125,000 jobs in our state. That’s 125,000 working people who won’t be able to provide for their families anymore. Unemployment means bills will start piling up, families will go hungry, and people will be forced to move from their homes. How is it okay to cost people their jobs, their care, their lives?
We’ve already seen this happen in our state. In the last decade, eight hospitals have closed in Kansas. In Fort Scott, the closure of Mercy Hospital devastated their town. Dozens of residents lost their jobs. People were forced to drive hours for care. School football games no longer had an ambulance on stand by. It wrecked their sense of stability.
Now imagine that multiplied by 100. That’s what we’re looking at with the passing of the “Big Beautiful Bill.” Thousands of people losing their jobs, communities becoming ghost towns, and Kansans dying due to lack of care- all to make the wealthy even richer. People in rural communities deserve as high quality of care as anyone else in the country, and it’s time that legislators start making the right decisions to ensure that no rural life is undervalued.
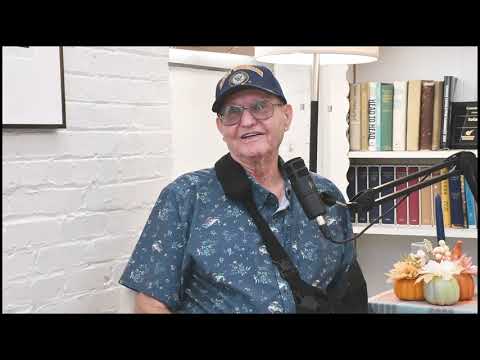
About the author: Jennifer Bacani McKenney, MD, FAAFP, is a family physician in her hometown of Fredonia. She has owned and managed her practice Fredonia Family Care since 2009.